Tarsal Tunnel Syndromes:
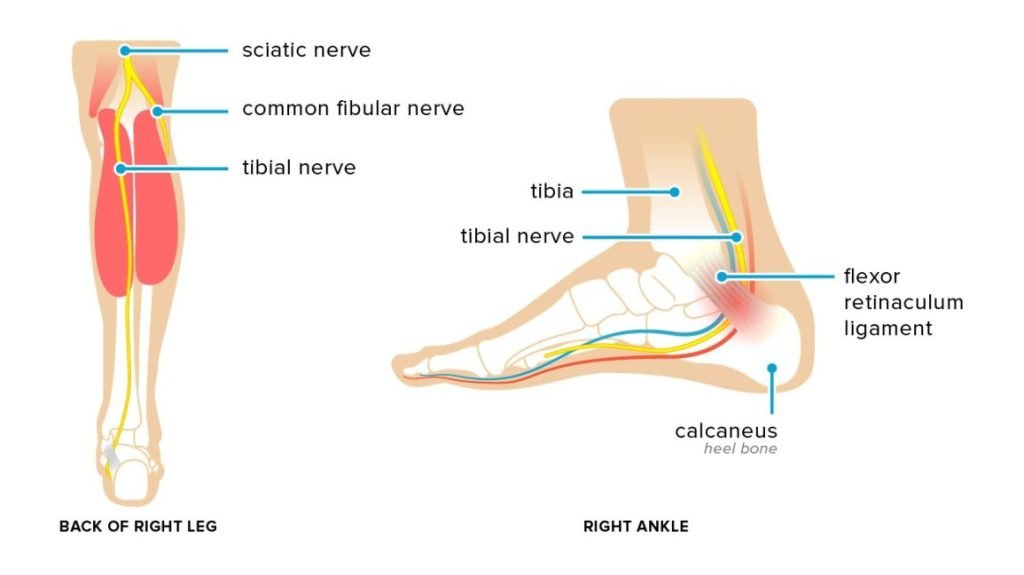
The tarsal tunnel is located on the inside of the ankle, and is formed by the ankle bones and the band of ligaments that stretches across the foot. Many of the blood vessels, nerves and tendons that provide movement and flexibility to the foot travel through the tarsal tunnel.
Tarsal tunnel syndrome (TTS) is caused by compression of the posterior tibial nerve as it travels through the tarsal tunnel. Compression of the posterior tibial nerve can cause pain, tingling or numbness in the foot.
Symptoms of Tarsal tunnel Syndrome:
People with tarsal tunnel syndrome may experience pain, numbness, or tingling. This pain can be felt anywhere along the tibial nerve, but it’s also common to feel pain in the sole of the foot or inside the ankle. This can feel like:
- sharp, shooting pains
- pins and needles
- an electric shock
- a burning sensation
Symptoms vary greatly depending on each individual. Some people experience symptoms that progress gradually, and some experience symptoms that begin very suddenly.
Pain and other symptoms are often aggravated by physical activity. But if the condition is long-standing, some people even experience pain or tingling at night or when resting.
Cause of Tarsal tunnel Syndrome:
Tarsal tunnel syndrome results from compression of the tibial nerve, and it’s often caused by other conditions.
- severely flat feet, because flattened feet can stretch the tibial nerve
- benign bony growths in the tarsal tunnel
- Varicose Veins in the membrane surrounding the tibial nerve, which cause compression on the nerve
- inflammation from arthritis
- lesions and masses like tumors or lipomas near the tibial nerve
- injuries or trauma, like an ankle sprain or fracture — inflammation and swelling from which lead to tarsal tunnel syndrome
- diabetes, which makes the nerve more vulnerable to compression
Tarsal Tunnel Syndrome Diagnosis:
Proper diagnosis of TTS requires the expert attention of experienced neurologists or Physiotherapist. It is important that the doctor determine the severity of the condition in order to recommend the most appropriate treatment plan, including Physiotherapy, Medication and surgery, if necessary.
A diagnostic workup for TTS may involve:
- A comprehensive clinical exam
- Complete medical history
- Electrical testing ( EMG or nerve conduction study)
- Imaging ( X-ray, CT scan or MRI)
Treatment Plan:
We recommend the following ways to treat and manage TTS according the Assessment:
- Rest: People can avoid using and putting pressure on the affected area as much as possible to prevent further damage and promote healing.
- Ice: A person can apply an ice pack wrapped in a cloth to the foot for 20 minutes. Leave the ice off for at least 40 minutes before repeating as necessary.
- Over-the-counter pain and anti-inflammatory medicatication.
Physiotherapy:
Physical therapy exercises may help reduce TTS symptoms by slowly stretching and strengthening the connective tissues, mobilizing the tibial nerve, and opening the surrounding joint space to reduce compression.
Types of physical therapy to treat TTS may include:
- Ultrasound therapy
- Acupuncture
- manual therapy(Mobilizing and Stretching Exercise)
- taping or bracing
- exercises to strengthen the tibialis posterior muscle
In severe cases of TTS or cases that do not respond to other therapies, people may require surgery.
Advice:
Orthopedic devices and corrective shoes: Podiatrists can make specialized shoes and inserts that help support the arch and limit motions that further irritate the inflamed nerve and surrounding tissues. Shoes also exist to help prevent pronation or inward rolling of the foot.
Reducing foot pressure: In some cases, wearing supportive shoes and socks may help reduce pressure around the foot. People with flat feet, severe symptoms, or nerve damage may require a brace to reduce pressure on the injured foot.
